Medical Fraud Detection in Python Projects
Medical Fraud Detection in Python Projects
Medical Fraud Detection in Python Projects
Abstract
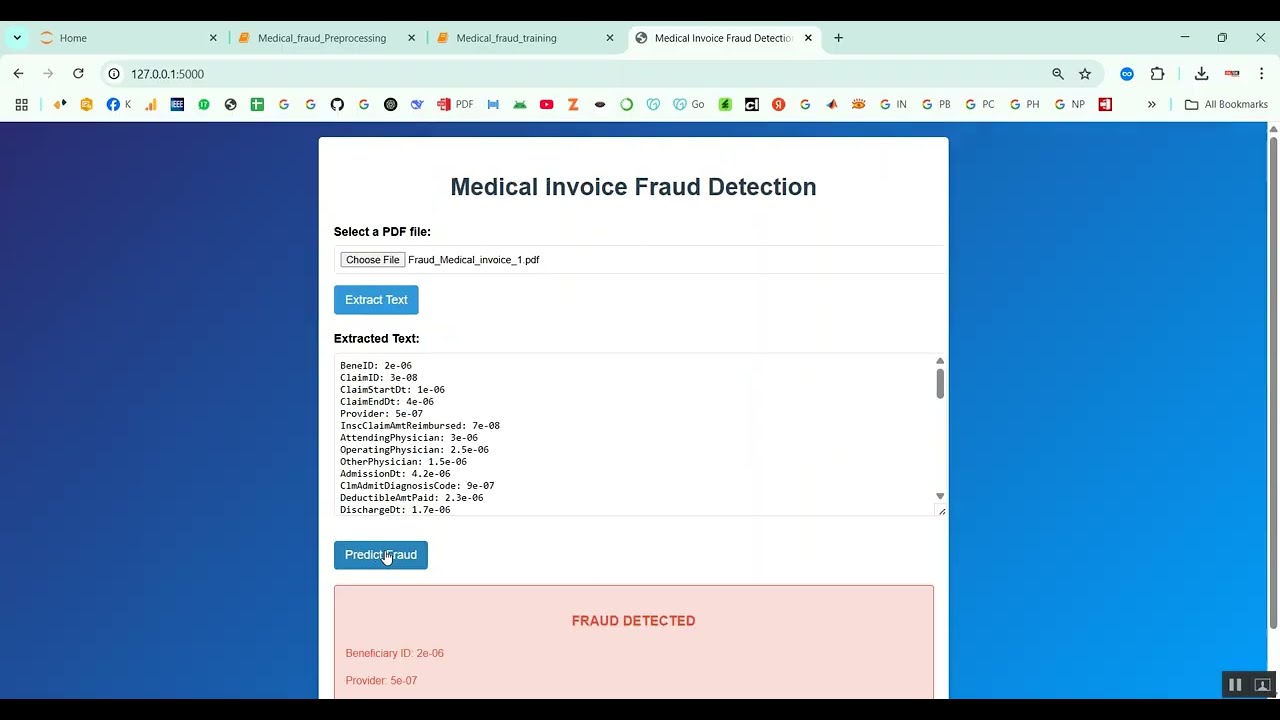
Medical fraud, including false claims, overbilling, and insurance scams, poses significant financial and operational challenges for healthcare systems worldwide. The project Medical Fraud Detection in Python Projects focuses on developing an intelligent system to detect fraudulent activities using machine learning and data analytics. Python is used as the development platform because of its robust libraries for data processing, analysis, and machine learning, including Pandas, NumPy, Scikit-learn, TensorFlow, and Keras. The system collects healthcare transaction data, patient claims, and billing records, applies preprocessing and feature engineering, and then uses predictive models to classify transactions as legitimate or fraudulent. By automating fraud detection, the system helps reduce financial losses, ensures compliance, and improves operational efficiency in healthcare organizations.
Existing System
Existing fraud detection systems in healthcare often rely on manual audits, rule-based checks, and predefined threshold alerts. While these methods can identify some fraudulent patterns, they are labor-intensive, slow, and unable to adapt to evolving fraud tactics. Traditional statistical approaches detect anomalies using simple metrics, but they often generate high false-positive rates and fail to capture complex patterns across multiple data dimensions. Moreover, manual review and conventional systems cannot scale efficiently to handle large volumes of healthcare transactions, leaving the system vulnerable to sophisticated fraud schemes.
Proposed System
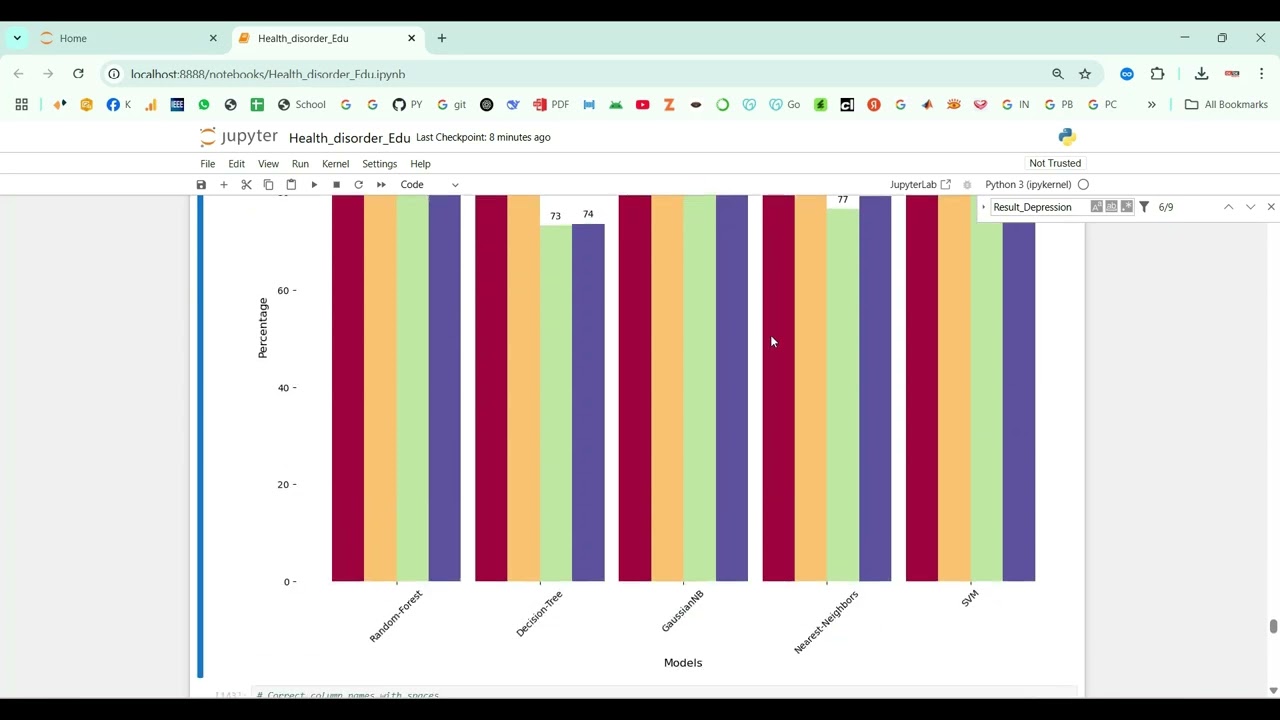
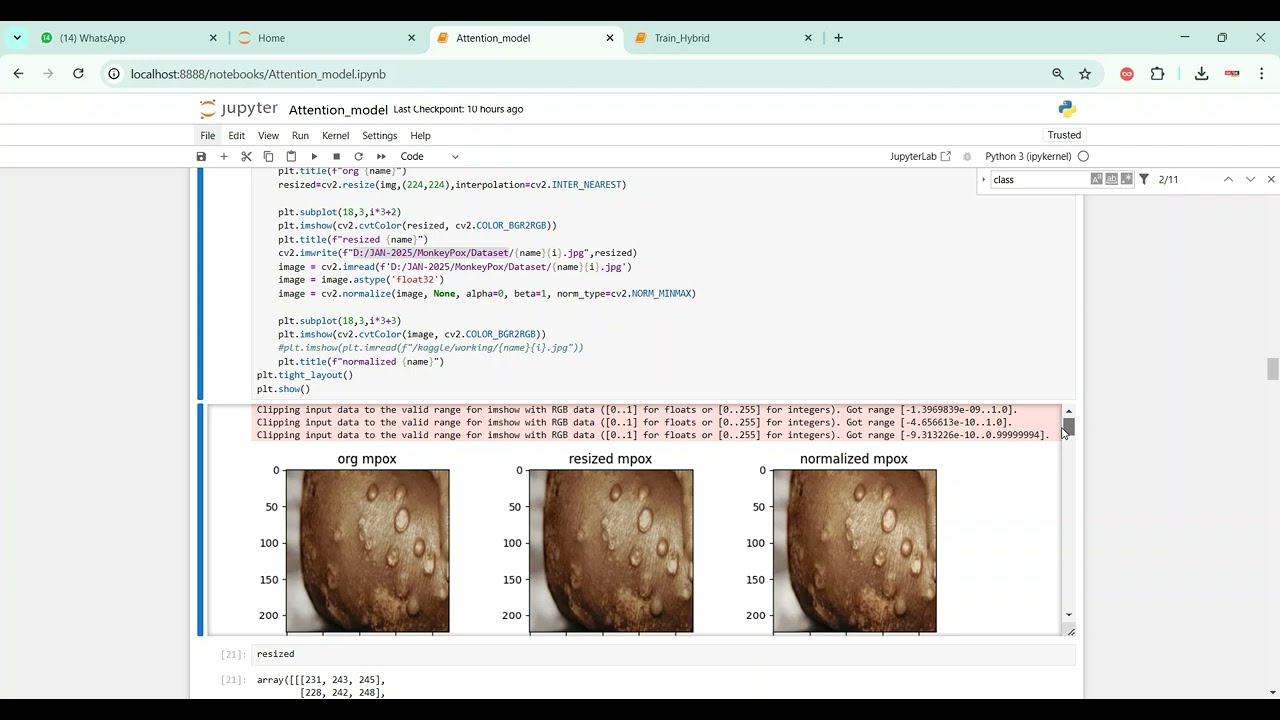
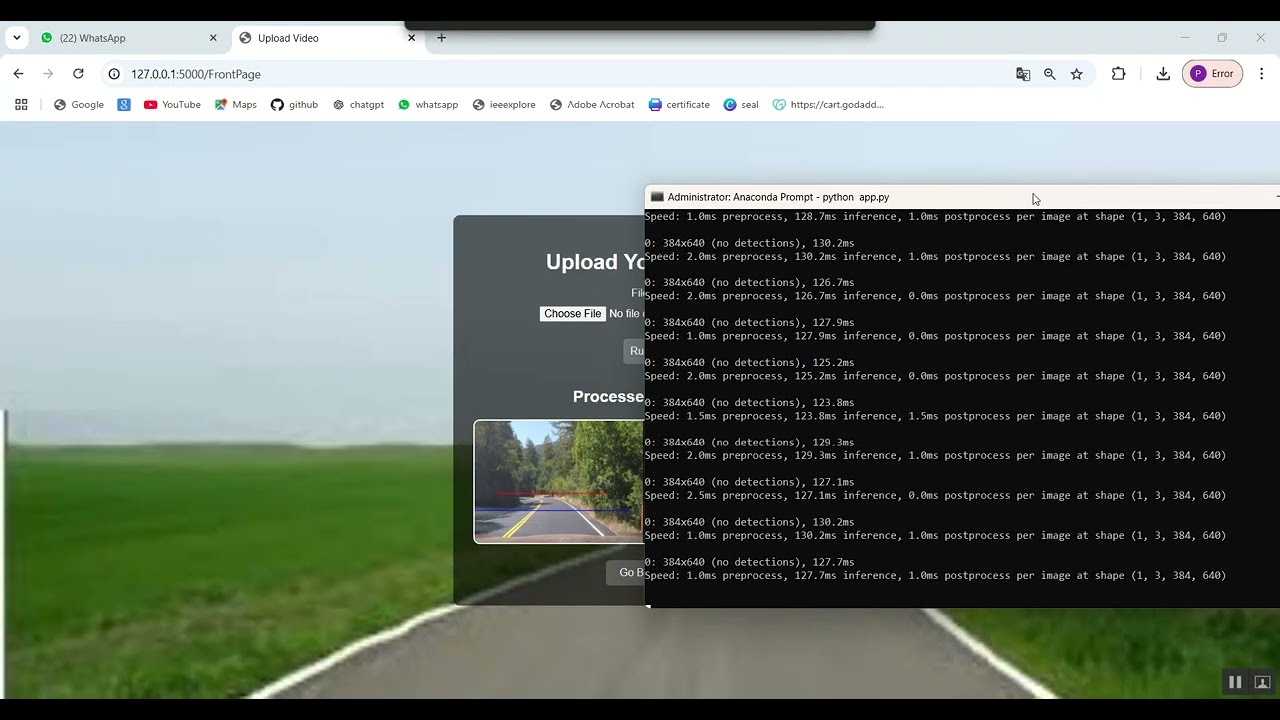
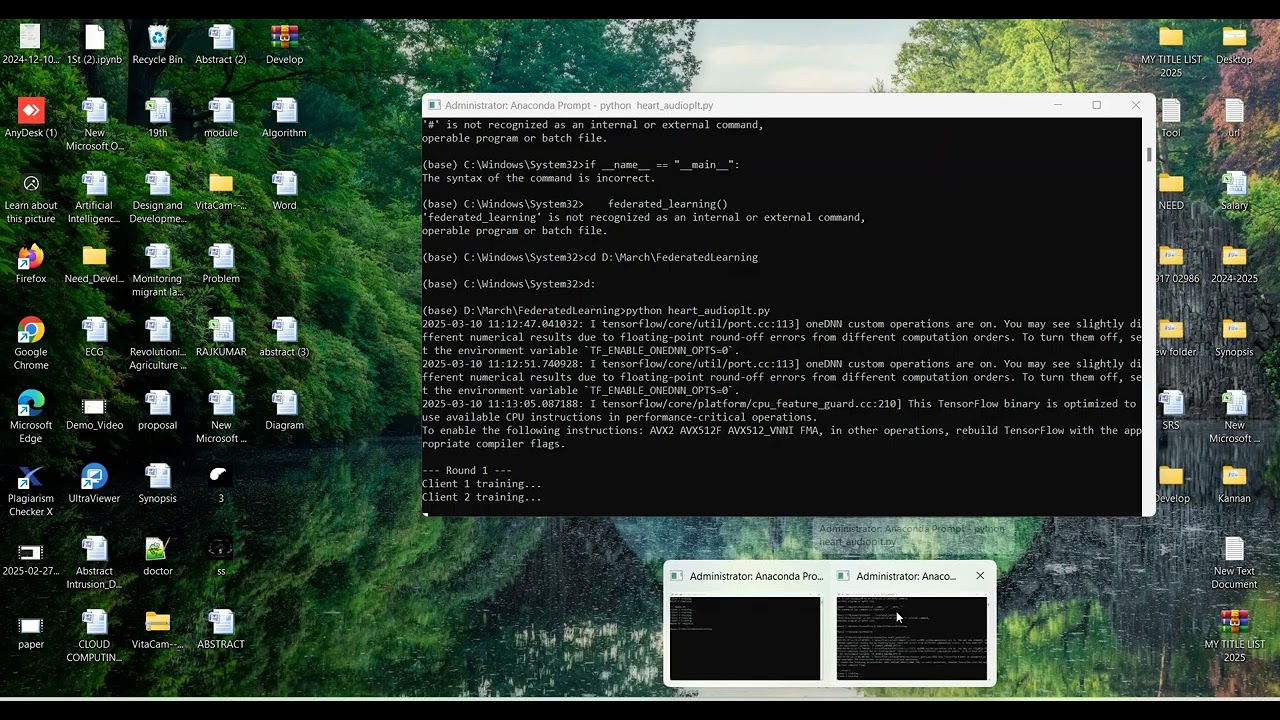
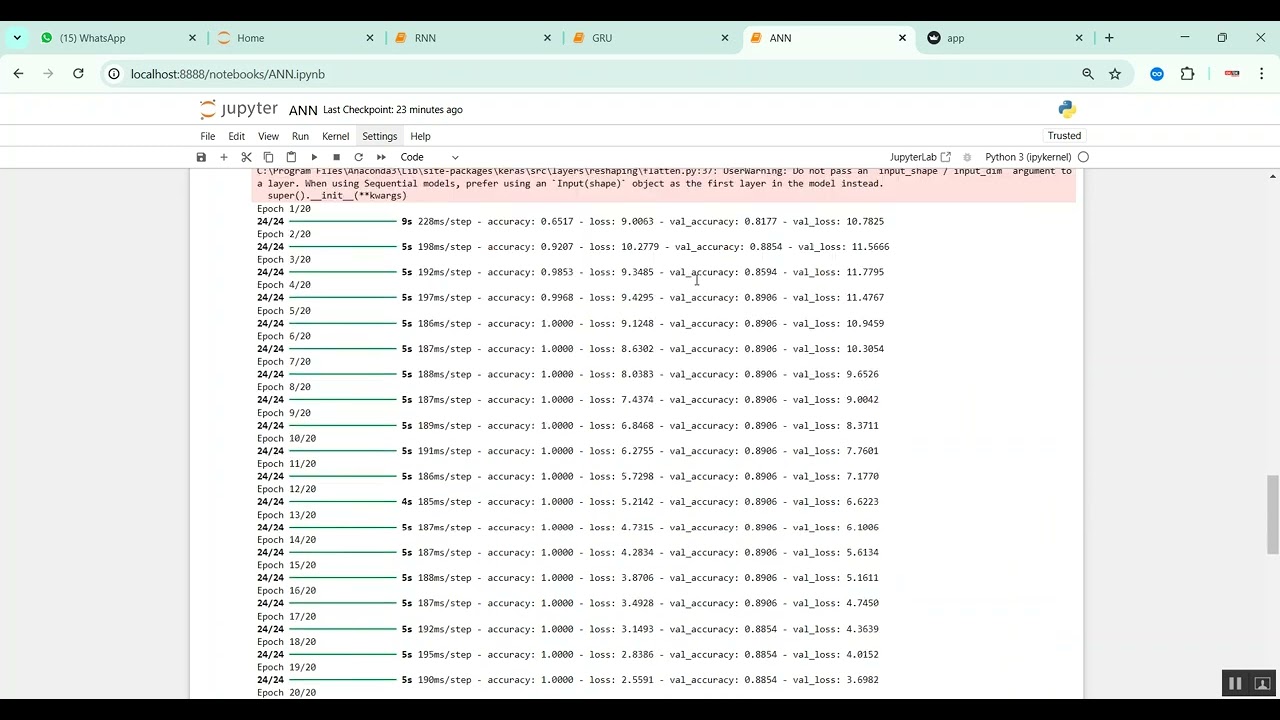
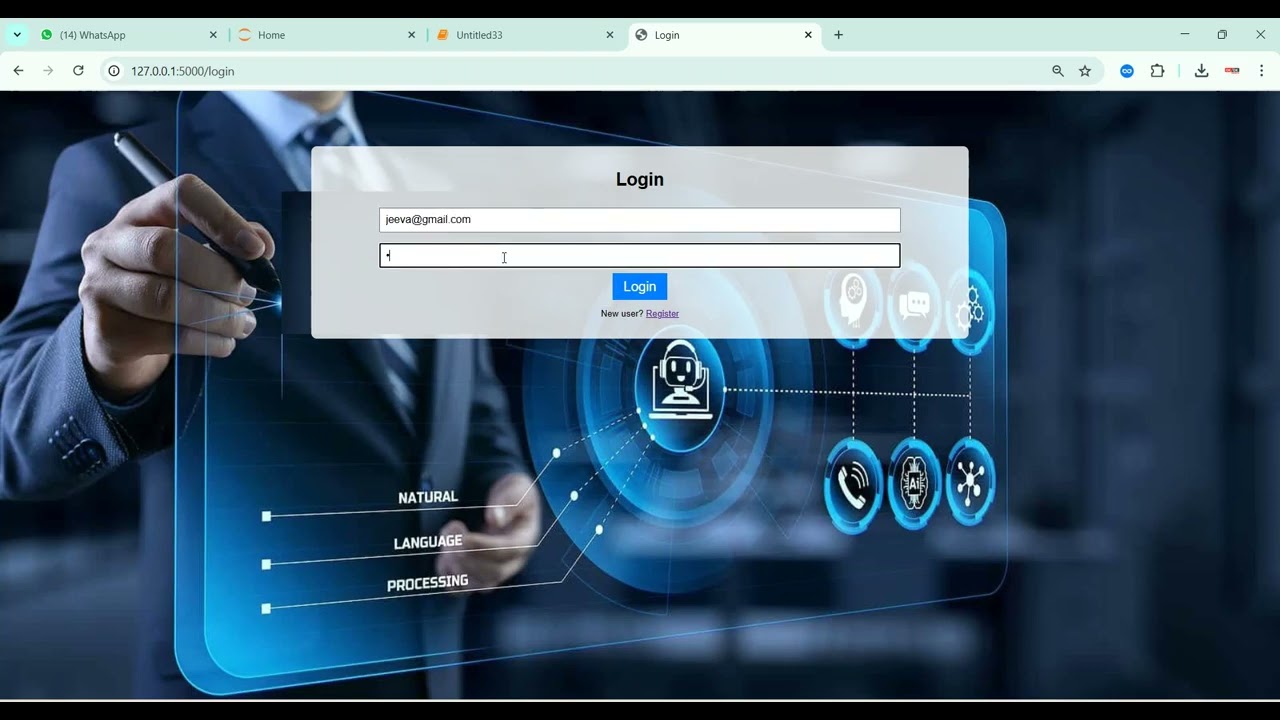
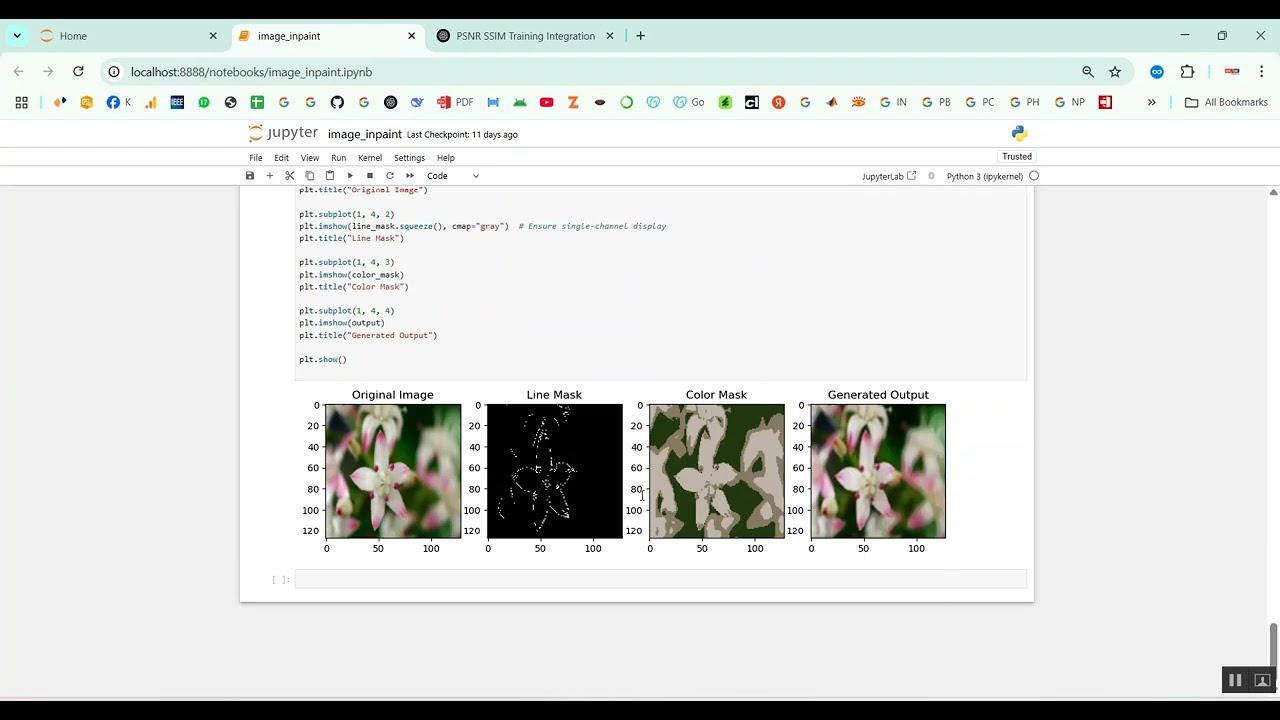
The proposed system introduces a Python-based machine learning framework for automated medical fraud detection. Healthcare data, including patient claims, billing records, and treatment codes, is preprocessed to handle missing values, normalize numeric features, and encode categorical variables. Feature engineering is applied to extract patterns indicative of fraudulent behavior, such as unusual claim amounts, abnormal procedure frequencies, or inconsistent patient histories. Supervised machine learning models such as Random Forest, Gradient Boosting, Support Vector Machines (SVM), and deep learning models like Artificial Neural Networks (ANN) are trained to classify transactions as legitimate or fraudulent. Performance evaluation is conducted using metrics such as accuracy, precision, recall, F1-score, and ROC-AUC. By integrating data-driven detection, real-time analysis, and predictive modeling, the system provides an efficient, scalable, and adaptive solution for identifying fraudulent activities in healthcare, reducing losses, and supporting regulatory compliance.
What's Your Reaction
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0